Researchers study how cancer cells repair their DNA, regulate their genes, differentiate, migrate, and recruit blood vessels in order to uncover both the mechanisms of disease as well as identify new therapeutic targets. This work is often conducted collaboratively, with clinicians providing insights from patients and basic scientists studying the molecular and cellular basis of the disease. At the same time, they also investigate existing therapeutics to identify factors that may predict which patients are most likely to benefit and to determine how their application might be improved.
Cell and cancer biology
Researchers
Adam Rudner
The Rudner laboratory focuses on understanding fundamental problems of chromosome dynamics. Defects in chromosome structure and segregation can lead to chromosome loss and damage, both critical events in the development of cancer and chromosomal disorders.
Barbara Vanderhyden
The Vanderhyden lab studies many aspects of ovarian cancer, including the role of specific genes in human ovarian cancer initiation, progression, chemo-sensitivity and prognosis. They create model systems of ovarian cancer to study disease initiation and to test the therapeutic efficacy of novel anti-cancer drugs. They are particularly interested in the role of stem cells in the ovarian and oviductal epithelia and their contribution to cancer initiation. With a growing interest in chromatin remodeling proteins, they are exploring the roles of these proteins in reproductive tissues, including ovary, placenta and embryonic stem cells.
Christine Pratt
NF-κB has critical roles in normal organogenesis, the immune system and cancer. Research in Dr. Pratt’s lab over the past several years has focused on the role that NF-κB plays in various forms of breast cancer. To study this, she utilizes both mouse models and mammary epithelial and tumor cell lines to dissect relevant signaling pathways.
Derrick Gibbings
RNA is not just the intermediate between DNA and protein. RNA acts as a post-transcriptional regulator, enzyme and ligand. In these multiple roles, RNA has critical impacts in cancer, neuromuscular disease and viral infection. The broad theme of Dr. Gibbings’ research program is to understand how RNA is regulated in the context of a complex cellular environment. Often, for simplicity, we portray processes involving RNA as occurring in a cytoplasmic void governed by random encounters. The lab aims to understand the complex life of RNA in a dense cellular milieu interacting with vesicles, organelles and regulatory complexes in the context of disease.
Douglas Gray
The central interest of the Gray laboratory is the regulation of protein stability and how a decline in proteolytic efficiency contributes to age-related diseases such as cancer and neurodegeneration. One area of particular interest is the role of deubiquitinating enzymes such as USP4 (which was discovered in the Gray laboratory), and the closely related enzymes USP15 and USP11. These enzymes have documented roles in different malignancies, and we are studying the evolution of this gene family in an attempt to determine how their substrate specificities arose.
Jean-Simon Diallo
Dr. Diallo is an Associate Scientist at the OHRI working with a multidisciplinary network of collaborators, he and his team are using medicinal chemistry, mass spectrometry and high-throughput molecular biology approaches to study how “viral sensitizer” drugs work. He is also expanding the scope of application of viral sensitizer drugs, which in addition to oncolytic virotherapy, show tremendous promise in virus/vaccine manufacturing and gene therapy applications.
John WR Copeland
Dr. Copeland’s laboratory investigates the role of the formin family of cytoskeletal remodeling proteins in governing cellular dynamics. Current projects focus on the role of FMNL2 in melanoma metastasis, the role of formins in cell-cell junction formation in endothelial cells, and the role of the novel formin INF1 in Golgi and primary cilium assembly
Jonathan Lee
The lab is broadly interested in breast cancer and the molecular biology of cell motility. To study these processes we use state-of-the-art technologies: bioinformatics, proteomics, high-resolution fluorescence microscopy, live cell microscopy and protein biochemistry to name a few. There are two ongoing research themes in the lab which include the remodeling of the actin cytoskeleton during cell migration and the role of the lipid kinase PI4KB in breast cancer.
Laura Trinkle-Mulcahy
Dr. Trinkle-Mulcahy is a cell biologist who uses a unique combination of fluorescence microscopy and quantitative proteomics to map the targeting of protein phosphatase complexes throughout the cell. These key enzymes contribute to the regulation of nearly all cellular signaling pathways; aberrant phosphorylation is a causative factor in a range of human diseases. A greater understanding of their regulation at the cellular level is thus essential for the development of therapeutic strategies targeted at these dysfunctional pathways.
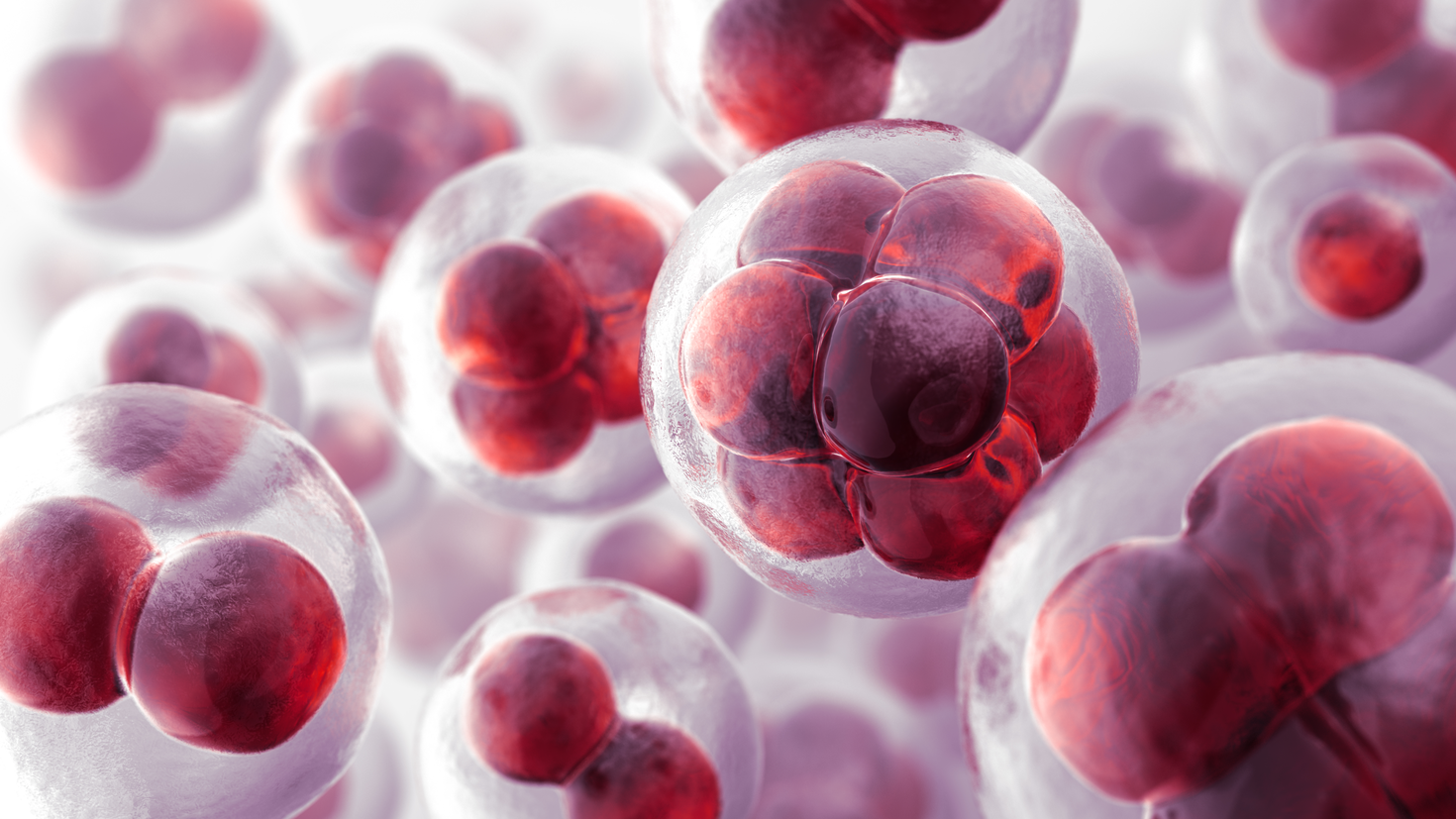
Lisheng Wang
Using cellular and molecular approaches and in vivo animal models, Dr. Wang’s laboratory is interested in nurturing human embryonic stem cells (hESCs) into mothers of circulatory cells and immune cells, generating transplantable cells for stem cell-based clinic therapy and reducing transplantation rejection. His laboratory is working on the targeting of embryonic signaling pathways in cancer for more effective treatment.
Ryan Russell
The Russell lab focuses on discovering the mechanisms underlying autophagy regulation in normal and pathological tissues. The autophagy pathway is the primary catabolic process in the cell, maintaining the integrity of organelles and the proteome. Additionally, autophagy promotes survival in response to depletion of cellular nutrients, DNA damage and hypoxia (low oxygen). Dysregulation of autophagy has been observed in several diseases including; cancer, Crohn’s disease and neurodegeneration.
Stephen Gee
The overall goal of Dr. Gee’s research program is to understand how lipid signals impinge upon the actin cytoskeleton to regulate fundamental cellular processes such as cell shape, movement and the uptake of nutrients. The lab’s main focus is the study of an enzyme called diacylglycerol kinase zeta (DGKζ), which phosphorylates the lipid second messenger diacylglycerol (DAG) to yield phosphatidic acid (PA), both of which have important signaling roles in cells. Dr. Gee’s lab is currently using a combination of biochemistry, cell and molecular biology, and advanced microscopic methods to study the role of DGKζ role in cancer cell migration, axon outgrowth and guidance, and skeletal muscle cell fusion and hypertrophy.
Tommy Alain
Surgery, chemotherapy and radiotherapy are the current standard-of-care treatments against cancer. A considerable number of cancers cannot be treated simply using the current available treatments. Scientists at University of Ottawa are working hard to devise new treatments based on an entirely different approach that involves the use of viruses to destroy human cancer. Dr. Alain laboratory is interested in understanding how these viruses modulate the gene expression of cancer cells thus contributing to the cancer demise. Gene expression is the cell’s program by which it synthesizes its various cellular components. We are currently investigating how oncolytic viruses modulate the gene expression program, specifically the process of mRNA translation.
Marjorie Brand
Dr. Brand’s research focuses on the regulation of gene expression at the level of transcription and chromatin/epigenetics. Her laboratory uses a combination of in vitro (proteomics, genomics) and in vivo (leukemia mice models, xenotransplantation of human leukemic cells in immunodeficient mice) approaches to understand how hematopoietic stem cells differentiate into blood cells and how deregulation of this process causes leukemia.
Kyle Cowan
Dr. Cowan's laboratory looks at the role of elastases, matrix metalloproteinases, and the extracellular matrix in the progression of pulmonary vascular disease associated with congenital diaphragmatic hernia. Dr. Cowan is also looking at the use of a stem cell approaches to treat pulmonary vascular diseasees associated with congenital diaphragmatic hernia as well as the role of pannexins in the regulation of skeletal muscle differentiation and tumourigenesis associated with rhabdomyosarcoma to identify potential new therapeutic targets
Chantal Matar
Dr. Matar’s research is focused on biomedical issues related to nutrition/immunology/cancer and how peptides and probiotics impact mucosal and tumoral immunity. Many aspects of the research involve in vivo assessments of immunomodulatory substances in mouse models and studying immunosurveillance against tumours and mucosal infections. Her lab is also specialized in analyzing biopeptide-mediated immune modulation in mucosal immunity, chemoprevention of mammary carcinoma and studying the molecular pathways involved in the immunopotentiating effect.
Lynn Megeney
Dr. Megeney’s lab studies the molecular mechanisms that control cell adaptation and cell differentiation. They are particularly interested in the biology of cell death proteins and how these factors are redeployed to promote these beneficial cellular functions. Dr. Megeney’s laboratory has focused on the role of the pro-death caspase protease family, a group of enzymes that target and cleave a large number of protein substrates. They utilize a broad range of model systems to interrogate caspase biology including yeast, mammalian cell culture and transgenic animal studies. Their long-term goals are to identify the constraints and substrates that allow caspase enzymes to promote stem cell maturation (differentiation) and act as beneficial remodeling agents during cell stress.
Luc Sabourin
The Sabourin laboratory is looking at the role of the Ste20-like kinase (SLK) in cancer cell motility. His research also focuses on understanding how much growth factor receptors, such as ErbB-2 (overexpressed in 25-30% of human breast cancers) and c-Met are coupled to extracellular matrix signaling and to the migration machinery using transgenic models and cell culture systems. He believes that delineating the molecular mechanisms translating growth factor signals to the migration machinery is key in the development of additional therapies targeted at the invasive potential of these tumors.
Duncan Stewart
The Stewart Lab is focused on translational research utilizing stem/progenitor cells for the treatment of cardiopulmonary and vascular diseases, together with enhancement strategies to increase their regenerative activity and overcome the deleterious effects of aging and attendant cardiac risk factors. Ongoing projects range from basic science discovery research on novel mechanisms of pulmonary hypertension and the role of exosomes in mediating the therapeutic effects of stem cells in vascular disease, to translational research including clinical trials on gene-enhanced progenitor cell therapy for acute myocardial infarction and immunomodulatory cell therapy for septic shock. The role of endothelial factors, such as nitric oxide and angiopoietins, in vascular health and disease, as well as angiogenesis and neovascularization, continues to be a central focus for Dr. Stewart’s laboratory.
Yannick Benoit
Dr. Benoit’s laboratory aims to describe the fundamental epigenetic phenomenon governing stem cell identity in the human intestinal epithelium and colorectal tumours. One of the main goals of the laboratory is to develop novel, anticancer agents targeting key epigenetic features of colorectal cancer stem cells. Moreover, Dr. Benoit aims to tackle the barrier of knowledge regarding the physiological role of chromatin organization in human intestinal stem cell identity and dynamic plasticity.
Damien D’Amours
Dr. D’Amours’ research program looks at the mechanisms that control cell cycle progression and genome stability in eukaryotes. In particular, we aim to reveal how cells divide their genome during mitosis and how they repair their chromosomes in the presence of DNA damage. His laboratory uses cutting edge proteomics and genomics analyses to identify novel effectors of chromosome stability and regulator of cell cycle checkpoints. Using a systems biology approach, our laboratory has provided critical new insights into the mechanisms responsible for the maintenance of genome integrity in health and disease states with a particular focus on the genesis of cancer and its resistance to chemotherapy.
Christina Addison
Dr. Addison’s research program focuses on two main themes; 1) the role of the tumour extracellular matrix (ECM) microenvironment in modulating tumour growth and angiogenesis and 2) cancer biomarker discovery. Her laboratory actively investigates the role of the ECM in modulating the growth of tumours and their response to common anti-cancer treatments. As the ECM present in tumors is vastly different than that found in normal tissue counterparts, understanding the effects of ECM on endothelial cell and tumor cell biology is extremely important. To this end she is also investigating the molecular events responsible for this modulation including the role of focal adhesion kinase and integrin linked kinase signal transduction pathways.
Rebecca Auer
Despite the removal of the solid tumor, such as colon cancer, the cancer will come back after surgery, often spreading to distant organs. Owing to physiological stresses incurred to the tissues during surgery, it is recognized that such procedures induce the spreading of cancer. Many patients get toxic treatments, such as chemotherapy, many weeks after surgery to try and prevent this. Dr. Auer’s research is focused on trying to understand why tumour cells spread after surgery and develop new approaches to prevent this.
John Bell
Dr. Bell’s research program is directed towards the identification and characterization of novel cancer killing therapeutic viruses that selectively infect and kill cancer cells, while leaving healthy cells and tissues unharmed. Not only did his laboratory discover and design these therapeutic viruses, but he also manufactures them for eventual clinical translation and commercialization.
Jim Dimitroulakos
Dr. Dimitroulakoslaboratory has two main research themes revolving around the identification of novel therapeutic approaches in the treatment of epithelial cancers including lung, head and neck and prostate carcinomas. The first research theme stems from the discovery that inhibiting the mevalonate pathway, involved in de novo cholesterol synthesis, can induce tumour specific killing. The second research theme is to identify novel mechanisms of action to common chemotherapies particularly the platin family of drugs. Although platins demonstrate activity in various tumour types, acquired or intrinsic resistance mechanisms limit their efficacy. One research project seeks to study a cellular stress pathway regulated by the activating transcription factor 3 (ATF3) as a key regulator of platin cytotoxicity. Understanding the role of this pathway in regulating platin-induced tumour cell killing and developing drugs that target this pathway to enhance platin efficacy will have therapeutic benefit.
Robert Korneluk
Dr. Korneluk’slaboratory is investigating the role of the Inhibitor of Apoptosis (IAP) gene family in the regulation of programmed cell death, also known as apoptosis. His group is investigating the role of IAPs – in particular, XIAP, cIAP1 and cIAP2 – in the progression of cancer, and exploring the use of small molecular IAP antagonists for cancer treatment. A particular focus is on the use of small molecular antagonists to enhance cancer treatment. His laboratory is also investigating the roles of the IAPs in muscle biology and disease. These studies will add insight into normal and disease processes involved in myogenesis and muscle repair in wasting syndromes such as muscular dystrophy, atrophy and cancer-induced cachexia.
Ian Lorimer
Dr. Lorimer’s research program revolves around the phosphoinositide 3-kinase pathway in cancer. His laboratory studies this pathway to identify and evaluate novel targets for cancer therapy. His recent work has focused on the role of protein kinase C; a protein initially known for its role in cell polarity and now also recognized for its role in promoting proliferation, invasion and resistance to chemotherapy in cancer cells. Currently a major focus of his lab is to characterize the role of the phosphoinositide 3-kinase pathway in tumour-initiating cells isolated from brain tumors.
David Stojdl
Cancer can be considered as the corruption of normal biological programs that control cell proliferation, metabolism, death, motility, stickiness and immune functions. Dr. Stojdl aims at harnessing the natural world of viruses to fight cancer. His laboratory designs and develops programmable replicating viruses called ‘oncolytic viruses’ as biotherapies that directly target cancer cells and activate a patient’s own immune system against their tumor.
Xiaohui Zha
Cholesterol is long known to be a necessary building block for mammalian cell membranes. In recent years, it is also widely appreciated that cholesterol plays a critical role in forming lateral membrane nano-domains. These domains facilitate protein/protein interactions, whereby providing central hubs for signal transduction. The focus of Dr. Zha’s laboratory is the study of cholesterol transport and membrane dynamics in mammalian cells. Her laboratory hopes to gain insights into the functions of cholesterol at the cellular level. Her laboratory employs novel biophysical and biochemical techniques to study these domains and link them to physiological cellular functions. Her lab currently focuses on one of the cholesterol transport proteins, ATP-binding cassette protein A1 (ABCA1); a protein for which mutations give rise to the Tangier disease.
Michele Ardolino
The immune system is an incredible weapon against tumors and yet, cancer is still one of the leading causes of death. It is of extreme importance to have a more detailed knowledge of the complex interactions between immune cells and cancer in order to design more tailored and effective immunotherapies. Dr. Ardolino’s group is interested in understanding why a subset of immune cells named Natural Killer (NK) cells are often able to kill tumor cells and to find new ways to harness the activity of NK cells against cancer. Currently, his lab is focusing on: 1. determining the functions of checkpoint receptors on NK cells. 2. understanding the cellular networks that suppress the NK cell response to cancer. 3. deciphering the molecular pathways responsible for suppressing NK cell activation in the tumor microenvironment.
Julie St-Pierre
The central research focus of the St-Pierre laboratory is understanding metabolic adaptation to physiological and pathological conditions. They are particularly interested in the plasticity of mitochondrial functions and how they contribute to overall energy homeostasis. Her team has contributed significantly to understanding the role of the master regulators PGC-1s in cancer, with a particular focus on poor outcome breast cancers. Her laboratory showed that PGC-1alpha plays a key role in setting the metabolic state of poor outcome breast cancers and that it promotes breast cancer growth. Recently, she is pursuing the investigation of the role of PGC-1s in breast cancer progression and other research projects on metabolic adaptations fueling metastasis and therapeutic resistance.
Areas of research
Stem cell biology and organismal development
Stem cells are precursor cells that have the capacity to self-renew